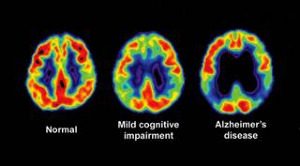
Researchers have determined the symptoms in human brain cells caused by the most common risk factor for Alzheimer’s disease: the Apolipoprotein E (APOE) gene. They also found a way to fix and erase the gene’s harmful effects.
The normal role of APOE is to provide instructions to create more proteins of the same name. With fats, APOE makes lipoproteins by binding lipids. The lipoproteins help transport and regulate the levels of cholesterol in the bloodstream. The APOE gene’s role in Alzheimer’s disease has been broadly studied. Researchers know that if a person has one copy of the 4th version of the APOE gene (APOE4), their risk of getting Alzheimer’s disease increases two to three times. Having two copies of the APOE4 gene increases the risk of Alzheimer’s disease 12 times.
Many studies show that APOE4 is damaging to the brain. Researchers at the Gladstone Institutes in San Francisco, CA, wanted to find out why, and get a picture of the critical difference between the third and fourth versions of the APOE variants that make the APOE4 gene so devastating. Is it that the fourth version is missing something that the third version has or that the fourth version has something that the third doesn't? Dr. Yadong Huang—lead investigator, and professor of neurology and pathology at the University of California, San Francisco—explained how important the question is:
“It’s fundamentally important to address this question because it changes how you treat the problem. If the damage is caused due to the loss of a protein’s function, you would want to increase protein levels to supplement those functions,” he said, “but if the accumulation of a protein leads to a toxic function, you want to lower production of the protein to block its detrimental effect.” In researching these questions, Dr. Huang discovered multiple drugs that worked well in mouse models--tests on mice with Alzheimer’s--but didn’t work in clinical trials--tests on human patients with Alzheimer’s.
So Dr. Huang and his team created neurons by applying stem cell technology to skin cells from people who had both, two copies of the APOE4 gene and Alzheimer’s disease, and from people who had two copies of the APOE3 gene but didn’t have Alzheimer’s disease.
Using these human neurons, the researchers found that the APOE4 protein has an abnormal form that prevents it from functioning properly. This then leads to a series of disease-causing problems.
Afterward, Dr. Huang, along with his team, wanted to learn if it was losing APOE3 or getting APOE4 that caused the disease. To find out, they compared neurons that didn’t produce the third or fourth versions of APOE with cells that had APOE4 cells added to them. The neurons continued to function normally until APOE4 was added, leading to Alzheimer’s-like pathologies. This confirmed that having APOE4 is what causes Alzheimer’s disease.
Lastly, the researchers looked for ways to redesign the gene. They applied a “structure corrector” that changes the structure of APOE4 to act and behave like APOE3. Applying this to human APOE4 neurons corrected the defects, thus eliminating any signs of the disease, restoring normal cell function, and helping the cells live longer.
In conclusion, the researchers said, “Treatment of APOE4-expressing neurons with a small-molecule structure corrector ameliorated the detrimental effects, thus showing that correcting the pathogenic conformation of APOE4 is a viable therapeutic approach for APOE4-related [Alzheimer’s disease].” Although this treatment for brain cells does not mean there is a cure for Alzheimer’s disease, it means that researchers are a step further to finding one soon.
[Source:
Medical News Today
]